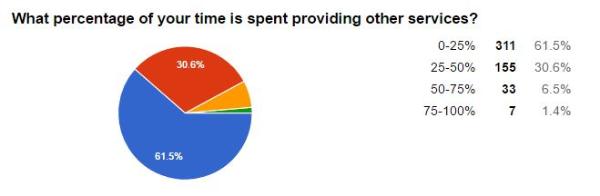
QUESTION #1: Are you a pediatric OT/COTA, PT/PTA, Parent, Teacher or other? (507 total responses)
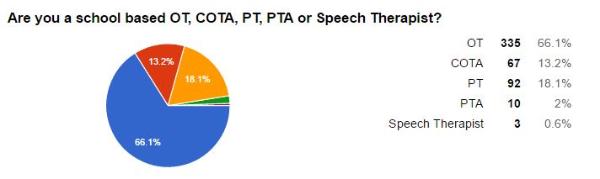
QUESTION #2: What percentage of your time is spent providing PUSH IN therapy services?
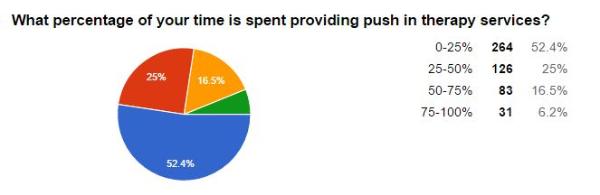
QUESTION #3: What percentage of your time is spent providing PULL OUT therapy services?
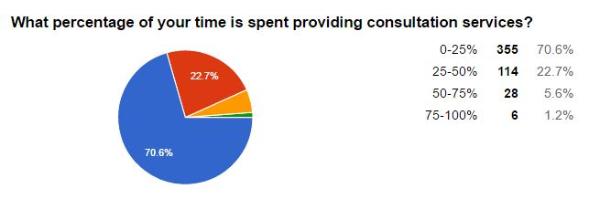
QUESTION #4: What percentage of your time is spent providing CONSULTATION services?
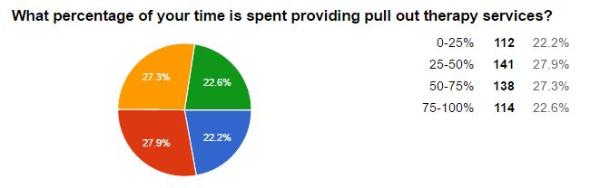
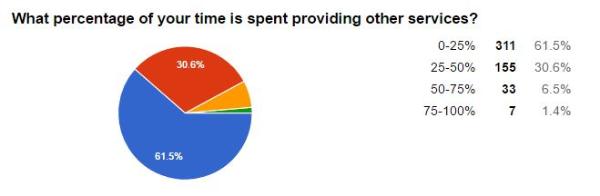
QUESTION #5: What percentage of your time is spent providing OTHER services?
SOME COMMENTS FROM RESPONDERS:
- paperwork for IEP’s, access, report cards, and evaluations/reevals vary from month to month. Heavy in the Spring with EI transition caseload.
- I prefer the carry over effect with push in services. The modeling that you do for the teacher and staff is more effective and provides quicker results.
- Paperwork takes a considerable amount of time and frequently do work at home on my own time.
- There is a lot of controversy within our district about what “consultation” is so I am thrilled that you are researching this and look forward to your results! questions: Does “consultation” require direct contact with the student? How do we build a measurable amount of time for consultation with students on the IEP? The way that I manage OT consultation with my students in my building is very flexible whereas other buildings in my district spend less time, unless it is required by the IEP.
- In our district, we have tried various times to push in to classrooms, but most teachers have been very resistant to this approach.
- We are trying to develop more opportunity for push-in services in our school, but I am finding out as a therapist that a lot of education towards teachers, paraprofessionals, and staff overall needs to take place first. Our role as OT’s needs to be clarified for some people, and it is my experience that teachers & staff tend to work inside their “box” and expect us to work inside ours. They are not understanding the true purpose of OT being in the classroom to support student functioning. Timing, schedules, class routines, and IEP goals all affect how successful a push-in session can be and it also makes a difference in the quality of the OT session sometimes as to whether the service is provided in the classroom vs. in the therapy room (based on staff collaboration, therapeutic tools available, and timing).
- Our department is now a fee for service provider. Therefore, we have to have 80% productivity (direct service) per day. We are no longer allowed to recommend consultation. A majority of paperwork has to be done “off book”.
- consultation time is not good use of time, especially when students need items-we don’t have enough time to get the items & then take back to the students I think in general we just don’t have enough time for all the “job” entails to be effective!!!
- We do not have consult services at this time. All services need to have direct face to face contact with the student therefore it’s considered direction. I also do a lot of RTi to support all kids in the classroom.
- There are several ways to look at time. My allocation is different at different times of the school year.
- I work with preschool students–most with autism. My school-based clinic is a big selling point when having prospective parents visit our school. This, of course, means pull-out services. I also personally believe that 1:1 services, when possible, in a quiet setting separate from the classroom are the most beneficial form of service for young children with moderate to severe autism.
- Scope of public school based practice includes providing supports to regular ed teachers, school counselors and other support staff via OT observations and consultations, in addition to evaluations, participation in Intervention and Referral Services (I&RS) and 504 Planning meetings.
- There are opportunities (1-3x yr. to contribute to staff/parent in-services and participate in district wide professional development.
- There are weekly department (OT/PT) department meetings to keep abreast of district wide demands, department and professional development. Department meetings have been instrumental in growth and support with many aspects of our dept. such as developing forms, eval templates, using various eval tools, grant applications, SMART goals, securing therapy work areas, materials and equipment, using EB interventions for program growth, etc. etc. etc.
- It think it depends mostly on the caseload of students in which you are providing service. For example, students in regular education settings are typically pulled out in order not to disrupt the rest of class and work on individualized goals. Students in an ASD classroom are able to be seen for push in services during rotations through various stations and life skill tasks.
- As a PT it is much harder to “push in” —even going to the 25 minute PE classes often wastes so much time due to instructional time, classes being late, behavior issues with other students, etc. I do try to check students in different classes, PE, playground, etc.
- The services depend upon the needs as well as reception of the teachers regarding how the services are provided. Preschool and more severe caseload, services are push in and consultation.
- I have found that direct instruction (pull out) for younger children is more successful,but I also need a consultative component in order for the students to have success within the classroom. Printing handwriting sheets, providing classroom accommodations, and researching equipment and the latest and greatest research/methods is how I spend the rest of my time.
- work in school and could use more prep and paperwork time.
- Under the RtI model I feel pulled to be in a lot of places in 2 different buildings. I don’t mind the many hats but conflicts arise and treatments are cancelled due to various responsibilities.
- I am finding more time is being spent on paperwork than before due to the new regulations continually changing with state billing etc.. Sadly, this takes my time from my students.
- I provide in class services primarily for FMD students or multiple disability students. I only pull students to an OT work area in HS or middle school. I provide pull out services in areas around the school where special area teachers also pull out students to help with reading. Often these are small groups (1-3) from different classrooms. (73 students and counting…)
- I am designated to be on an early childhood evaluation team, which consists of 1.5 days/week. Other therapists in our district our not on this evaluation team.
- RtI or MTSS is influencing delivery style, goals and minutes. Questions about license and services without evaluations are big concerns.
- I wish I had more support for push in services!!
- I really want to push-in more, but there is such a focus on handwriting that it’s difficult to get to serve elsewhere (unless the student just has self-regulation issues, where I can have more flexibility). I think many teachers don’t really understand OT, other than what they’ve seen from other OTs that they’ve worked with…so as a new practitioner I feel uncomfortable telling an experienced teacher that they don’t understand (I’m working on this).
- The model that is used in my setting is the OTs supervise COTAs, complete all paperwork, attend meetings and collaborate as a team member.
