Postural Control, Gross Motor Development and Mealtime
When you think of children and mealtime, the first things that come to mind may be related to the hand and mouth – ie the ability to use a spoon or fork, bringing food to mouth and getting food inside the mouth. What you may not realize is that the child’s postural control and gross motor skills greatly influence the ability to function independently during mealtime. The hips affect the lips!
GROSS MOTOR SKILL DEVELOPMENT AND MEALTIME
Alignment of the mouth and jaw for feeding is interconnected to head and trunk stability. As babies develop their gross motor skills, they become developmentally ready to try solid foods. This is usually around 6 months of age when the baby is able to: sit with support in an upright position (either on the lap or in a suitable high chair), roll over, rotate trunk and head voluntarily and bring hands and toys to mouth for exploration.
As children begin to increase their mobility, they learn to position themselves independently during mealtimes in a variety of settings including on the floor, small tables and chairs or at the dining room table. At around 17-19 months, children can back into a small chair or slide sideways onto the chair to sit to eat at a small table. Around 18-21 months, children can climb forward onto an adult chair, turn around and sit. At around 37 – 46 months, children eat most foods without significant mess. Regardless of where they are seated, children need to have the postural control to remain upright and stable while eating not only to control oral motor skills but to prevent choking.
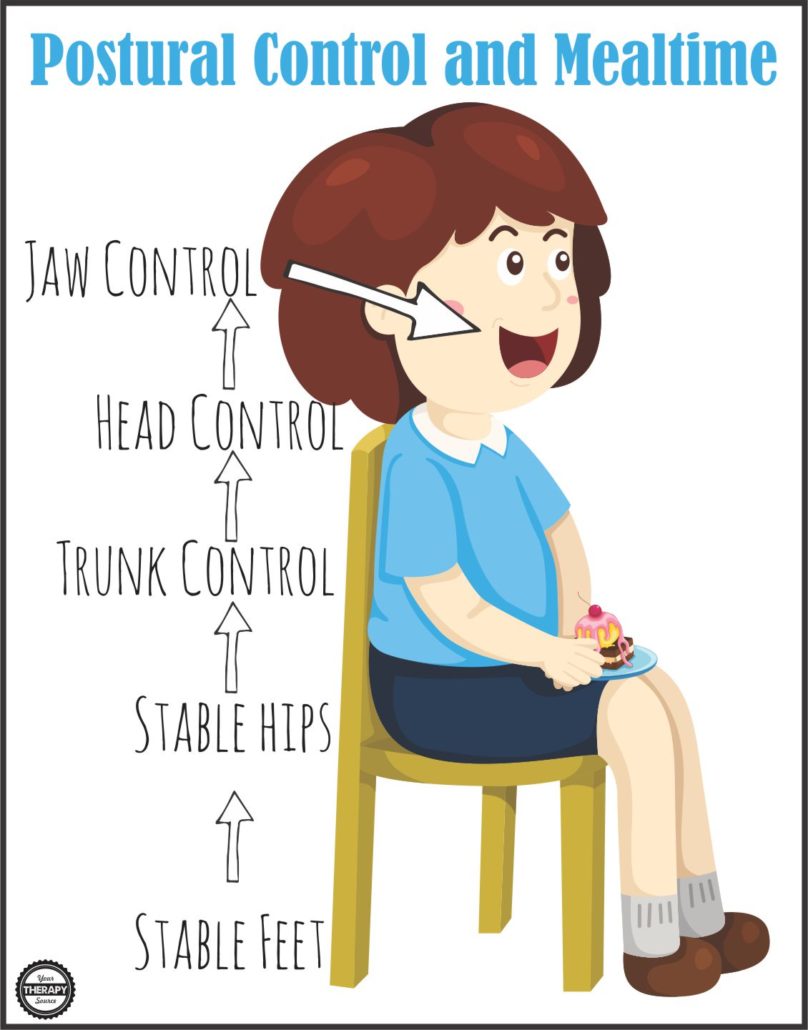
POSTURAL CONTROL AND MEALTIME
In order to achieve proper alignment of the head during mealtimes, the baby or child needs to be stable at the pelvis, trunk and head. Children with neurotypical development may be able to compensate with regards to oral motor skills if there is misalignment in the trunk. Children with disabilities, may exhibit significant difficulties with oral motor skills if there is a lack of postural control.
Starting at the pelvis, the hips should be stable, symmetrical and around a 90 degree angle. This stable pelvis will allow the child to maintain a more upright posture. Foot support can help to increase pelvic stability, therefore in the older child, the feet should be positioned on the floor or a foot stool. The sitting posture should be approximately 90 degrees at the hips, 90 degrees at the knees and ankles.
The trunk should also be symmetrical allowing the child to sit up straight during mealtime. For children with significant disabilities, adaptive seating may be necessary to achieve a stable pelvis and trunk.
Having a stable pelvis and trunk allows for proper head position for mealtime. Research indicates that a child’s head position influences the swallow during feeding and reduces the risk of aspiration. The recommended head posture for safe swallow is a “chin tuck.” The head is positioned upright, in midline, with slight neck flexion, so that the chin is directed slightly downward and inward. For children with significant physical disabilities, a caregiver may have to facilitate the position for safe swallowing.
GROSS MOTOR ACTIVITIES TO HELP WITH POSTURAL CONTROL FOR MEALTIME
Here are 5 gross motor activities to work on improving postural control to encourage pelvis, trunk and head stability for mealtime-
- Play in prone. Play any games while lying on your stomach, hands under shoulders, propped up on your elbows. This position helps to facilitate postural control and a chin tuck especially if game pieces, books, puzzles, etc are placed on the floor.
- Small weight shifts while sitting on an exercise ball. When you move back and forth or side to side on a therapy ball, very slowly and in control you are activating your pelvic and trunk muscles to keep your body stable.
- Animal walks or yoga poses. Try different animal walks or yoga poses that require activation of the trunk and hip muscles. For example, cat/camel pose, crab walking, bear walking, etc.
- Swinging. Maintaining your balance while pumping a swing requires a significant amount of postural control. Challenge the child’s postural responses by occasionally stopping and starting the swing. The child will have to activate their postural muscles to maintain upright.
- Add kneeling, squatting or sit to stand transfers to any activity. When you perform those actions you activate the hip and trunk muscles. Position toys so a child has to squat down to pick something up. Put toys a low table or bench and the child can kneel to play. Use vertical surfaces (ie whiteboard on a wall, magnetic wall, etc) so child has to sit to stand to complete the activity. Play Strong includes 40+ playful activities that encourage muscle strengthening in children.
This post is part of the Functional Skills for Kids series is on mealtime. This series is a 12-month long series written by occupational and physical therapy bloggers on the development of 12 functional skills for children. Stop by to see what the other occupational therapists and physical therapists in the Functional Skills for Kids series have written on mealtime.
When Can Kids Feed Themselves? (and other mealtime milestones) | Mama OT
Fine Motor Skills For Mealtimes | Therapy Fun Zone
Postural Control, Gross Motor Development and Mealtime |Your Therapy Source
Attention, Behavior, and Meal Time Problems | Sugar Aunts
4 Ways to Modify Meal Times for Fussy Eaters | Your Kids OT
Mealtime Skills, Rituals & Play – Nurturing a Love for Food | Kids Play Space
15 Tips for Picky Eaters | The Inspired Treehouse
Positioning, Motor Skills, and Table Manners: What the Connection? | Miss Jaime OT
Visual Perceptual Skills Needed for Independent Feeding | Growing Hands-On Kids
References:
Furano et al and Parks, S (2014). HELP® Checklist 0-3 Birth to Three Years. VORT Corporation.
Redstone, F., & West, J. F. (2004). The importance of postural control for feeding. Pediatric nursing, 30(2), 97.
Royal Children’s Hospital Melbourne. Physical, Sensory and Oral Motor Development. Retrieved from the web on 10/25/16 at http://www.rch.org.au/feedingdifficulties/development/physical-sensory-oral-motor-development/.
Teaford, P et al (2010). HELP® Checklist 3-6 Checklist. VORT Corporation.




Comments are closed.