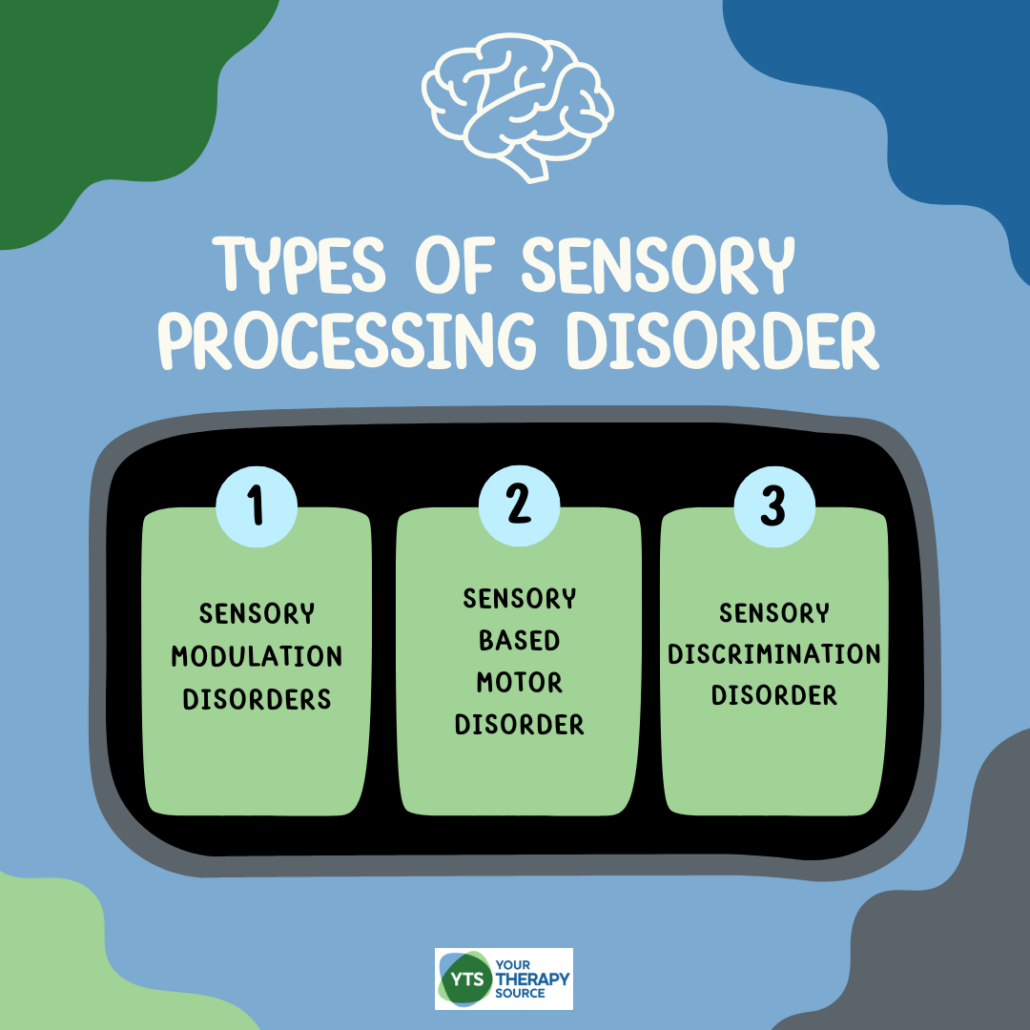
Types of Sensory Processing Disorder
Sensory Processing Disorder (SPD) affects how the brain interprets sensory information, making it difficult for individuals to respond appropriately to the world around them. For some, certain stimuli like loud noises or bright lights can feel overwhelming, while others might seek out intense sensory experiences, craving more stimulation than the average person. SPD is a complex condition, and understanding the different types can help parents, teachers, and occupational therapists provide better support for children struggling with sensory processing. Learn more about the main types of sensory processing disorder, how to help children manage their sensory challenges, and when it might be time to seek professional help.
WHAT IS SENSORY PROCESSING DISORDER?
Sensory Processing Disorder is a neurological condition where the brain has trouble receiving and responding to sensory input, leading to difficulties in everyday activities. It can result in sensory overload, sensory seeking, or poor motor coordination. Occupational therapy is often used to help children navigate these sensory challenges and function better in their daily lives.
Examples of SPD may include:
- Difficulty processing sensory input like touch, sound, and light
- Challenges with balance, coordination, and motor skills
- Sensory overload in environments with bright lights or loud noises
- Sensory seeking behaviors like constant movement or craving deep pressure
- Affects sensory systems such as vision, hearing, touch, and proprioception
Sensory Strategies Workbook
TYPES OF SENSORY PROCESSING DISORDER
SPD is classified into three main types, each with its own subtypes and symptoms:
Types of Sensory Modulation Disorders
- Sensory Over-Responsivity:
- Responds to sensory stimuli more intensely and for longer durations
- Symptoms include covering ears for moderate sounds, avoiding touch or messy play (sensory avoidance), and being overly sensitive to light and noise
- Common triggers: loud noises, physical contact, bright lights
- Sensory Under-Responsivity:
- Exhibits little or no response to sensory stimuli (low registration)
- May not feel temperature changes or respond to pain
- Appears withdrawn or passive; may seem “lost in their own world”
- Sensory Seeking:
- Constantly seeks intense sensory stimulation
- Always moving, crashing, or jumping; sometimes mistaken for ADHD
- Sensory input like spinning (vestibular input), crashing, or spicy foods may not satisfy sensory craving
Sensory-Based Motor Disorder
- Postural Disorder:
- Poor postural control, leading to poor balance and stability
- Weak muscle tone, slouching, and poor endurance are common symptoms
- Struggles to use playground equipment or maintain balance
- Dyspraxia:
- Difficulty planning and executing movements
- Problems with fine and gross motor skills, such as writing, dressing, or playing sports
- Decreased body awareness – has difficulty controlling their own body
- May be clumsy, frequently bumping into things
Sensory Discrimination Disorder
- Trouble distinguishing between different sensory stimuli
- Difficulty interpreting subtle qualities of objects, such as textures, shapes, or sounds
- Challenges include recognizing letters, sounds, or objects by touch
Sensory Lifestyle Handbook
EXAMPLES OF THE TYPES OF SENSORY PROCESSING DISORDER
Every student is unique, and when it comes to Sensory Processing Disorder, many children do not fit neatly into just one type. It’s common for students to display characteristics of multiple sensory challenges, which makes each child’s sensory profile distinct. For example, a student might be highly sensitive to loud noises while also seeking out tactile input through constant movement. The examples provided below offer a glimpse into how different types of sensory processing disorder might present in a classroom, but it’s important to remember that many students will show a combination of these behaviors or fluctuate in their responses depending on the situation. Understanding these differences helps teachers, parents, and therapists better support the individual needs of each child.
Examples of Sensory Modulation Disorder
- Sensory Over-Responsivity
- Example: Jenny is a 6-year-old who covers her ears during recess because the noise from other children playing is overwhelming for her. In class, she avoids participating in art activities that involve messy materials like finger paint because she is highly sensitive to touch. Bright lights in the classroom make her squint and seem uncomfortable, and she prefers sitting in the back of the room to avoid visual stimulation.
- Common Triggers: Loud noises during transitions, background noise, unanticipated physical touch from peers, or bright lights in a classroom.
- Sensory Under-Responsivity
- Example: Ethan is an 8-year-old who seems disengaged during class activities. His teacher often calls his name multiple times before getting a response. He doesn’t seem to notice when he gets small cuts or scrapes during recess, and he often doesn’t feel when his clothes are twisted or when the room is too hot or cold. Ethan appears passive and is frequently described as being “in his own world.”
- Common Presentation: A child’s behavior may appear sleepy, slow to respond, or unaware of their surroundings. They might not react to stimuli that others find uncomfortable, such as loud noises or physical discomfort.
- Sensory Seeking
- Example: Liam is a 7-year-old who constantly fidgets, jumps, and moves around the classroom. He loves to run and crash into things during recess, often leading to rough play with peers. Despite being asked to sit during lessons, Liam continuously gets up, taps his feet, or seeks out movement. In addition, he frequently chews on non-food items like erasers and pencil tops. His teacher often mistakes his behavior for hyperactivity or impulsivity.
- Common Presentation: Constantly seeking sensory input such as spinning, crashing, or touching everything around them. Their nervous system may find it hard to sit still or engage in quiet activities.
Examples of Sensory-Based Motor Disorder
- Postural Disorder
- Example: Sofia is a 9-year-old who has trouble sitting upright in her chair for long periods. Her teacher often finds her slouching or leaning on her desk during lessons. At recess, she avoids playground activities like climbing or balancing on equipment because she lacks the core strength and endurance needed for these activities. Sofia tires easily and struggles to keep up with her peers during physical activities.
- Common Presentation: Weak muscle tone, difficulty maintaining posture, struggles with balance and endurance during both classroom and recess activities.
- Dyspraxia
- Example: Oliver is a 10-year-old who has difficulty with tasks that involve fine and gross motor skills. In class, he struggles with writing legibly and often avoids tasks like cutting with scissors or drawing. During physical education, he appears clumsy and has trouble catching or throwing a ball. He often bumps into things, spills items, and takes longer to complete multi-step tasks like getting ready for gym class or following along in group dance or yoga activities.
- Common Presentation: May appear uncoordinated, struggle with motor planning, and have difficulty with both fine motor tasks (like writing) and gross motor tasks (like playing sports).
Examples of Sensory Discrimination Disorder
- Example: Ava is a 6-year-old who struggles with distinguishing between similar sounds in phonics lessons, making it difficult for her to differentiate between the letters “b” and “p.” During math, she has trouble identifying small differences between objects, which causes her to misinterpret shapes or struggle with sorting items by size. When asked to find her pencil in her desk without looking, Ava has difficulty identifying it by touch alone and often pulls out multiple objects before finding the correct one.
- Common Presentation: Difficulty interpreting subtle differences in sensory stimuli, leading to challenges in distinguishing sounds, recognizing letters, or identifying objects by touch.
These examples offer a snapshot of how various types of symptoms of sensory processing disorder that can manifest in the classroom. However, it’s important to recognize that each child may show a blend of behaviors from different types or subtypes, and their responses may vary depending on the environment or activity. Understanding these patterns enables educators and caregivers to provide more targeted support for children with sensory processing difficulties.
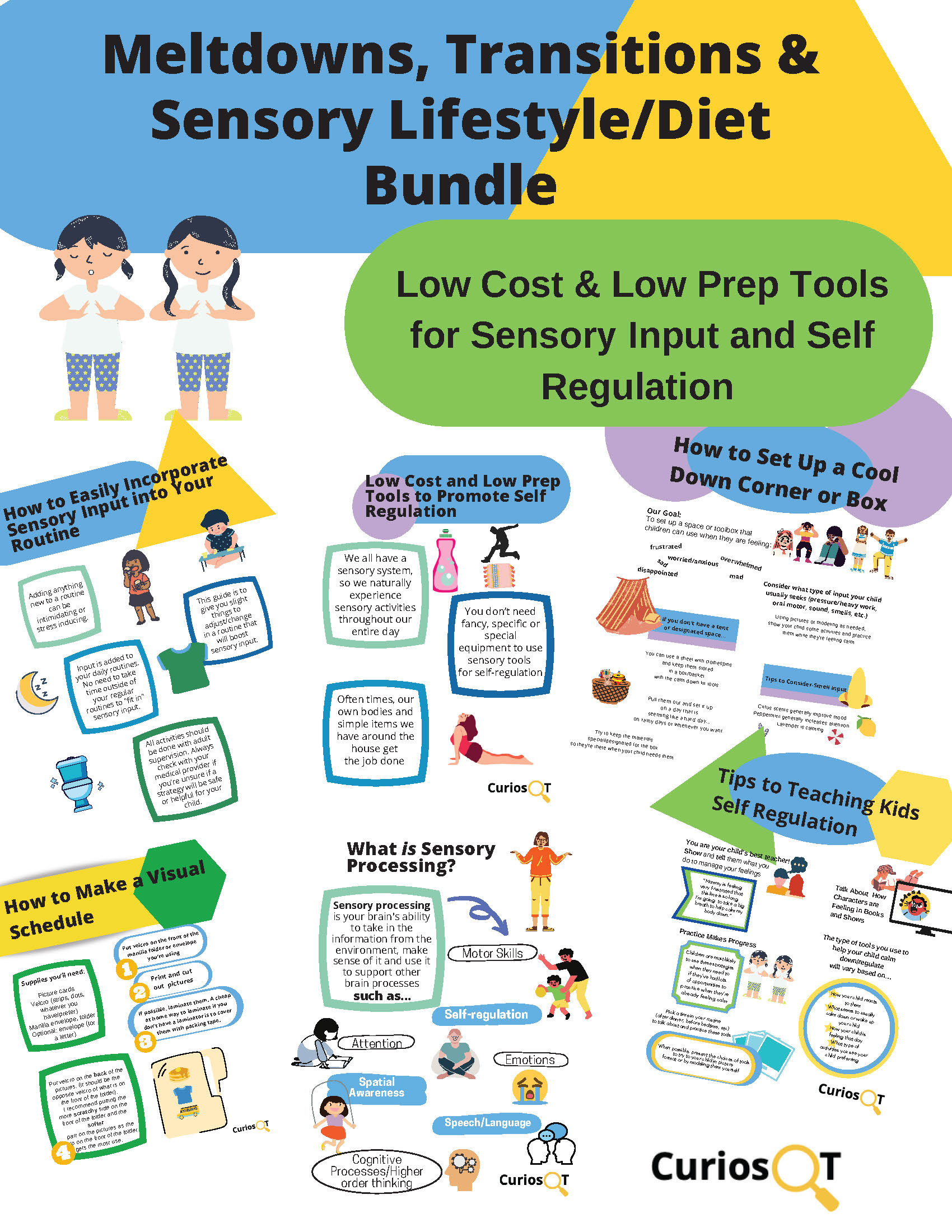
Meltdowns, Transitions, and Sensory Lifestyle Bundle
DIAGNOSTIC CRITERIA FOR SENSORY PROCESSING DISORDER
Sensory Processing Disorder (SPD) is not officially recognized as a distinct disorder in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Therefore, SPD can not be “diagnosed”. SPD is often identified through clinical observations and assessments conducted by occupational therapists or other specialists. These evaluations typically include observations of the child’s behavior in response to various sensory stimuli, parent or caregiver reports, and standardized tests such as the Sensory Profile or Sensory Processing Measure. To meet the criteria for SPD, a child must show consistent sensory-related difficulties that interfere with their ability to perform everyday tasks, including challenges with processing and responding to sensory information across multiple sensory systems, such as touch, sound, sight, and movement. The child’s sensory issues must also significantly disrupt their ability to function in environments like school or home, leading to challenges with social participation, academic performance, or daily living skills.
HOW TO HELP CHILDREN WITH SENSORY PROCESSING DISORDER
Children with sensory processing issues benefit from structured routines, sensory-friendly environments, and activities designed to meet their specific needs. Here are some ways to help:
- Sensory Strategies: Tailored activities that provide the right type and amount of sensory input (e.g., weighted blankets, sensory gyms).
- Occupational Therapy: Helps children develop coping strategies, improve motor skills, and manage sensory challenges.
- Modify the Environment: Reduce sensory triggers such as loud noises or bright lights. Create calming spaces where children can take breaks from overwhelming stimuli.
- Engage in Sensory Play: Activities like swinging, climbing, or deep pressure activities (e.g., using body socks, weighted vests) can help regulate the sensory system.
WHEN TO ASK FOR HELP
Parents should seek professional help if their child’s sensory processing problems interfere with:
- Daily life activities: Difficulty functioning at school, home, or in social situations
- Behavior: Extreme reactions to sensory input, meltdowns, or avoidance behaviors
- Mental health: Increased anxiety, frustration, or low self-esteem due to sensory challenges
A healthcare provider, such as an occupational therapist or physical therapist, can conduct evaluations and recommend treatment options, including sensory integration therapy and a sensory diet.
MORE HELPFUL RESOURCES
For more information on sensory processing and how to support children with SPD, explore the following resources:
- Learning Style and Sensory Processing
- Supporting Sensory Processing in Children with Autism
- Sensory Processing and Anxiety
- Sensory Classroom Ideas for All Students
- Autism and Sensory Processing Disorder
- Effortful Control
- Screen Time and Sensory Processing
REFERENCE:
Miller, L. J. (2014). Sensational kids: Hope and help for children with sensory processing disorder (SPD). Penguin.